Abstract
Background: Health Technology Assessment (HTA) is increasingly recognized as a critical tool for evidence-based health financing decisions in Sub-Saharan Africa. However, its adoption is influenced by a variety of factors. This study synthesizes evidence from the literature on the factors enabling and hindering HTA institutionalization in the region as a means of supporting universal health coverage (UHC).
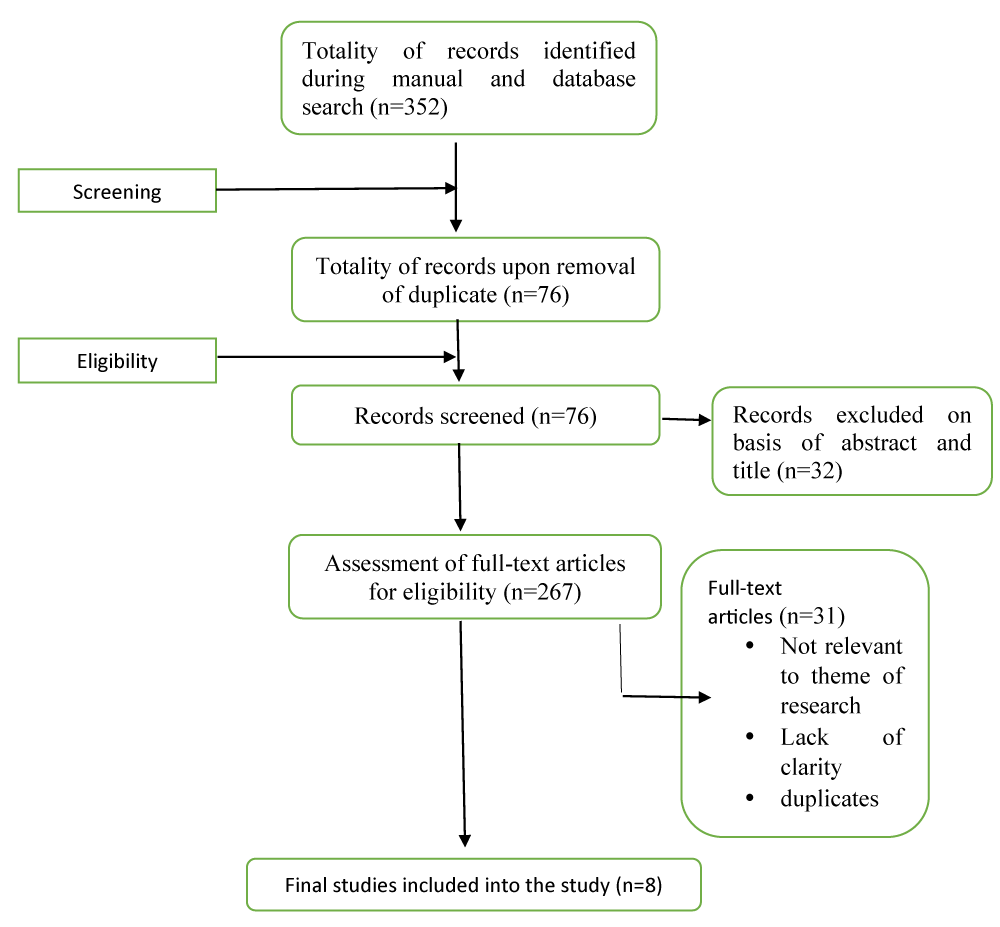
Methods: A systematic analysis of eight country-specific nonsystematic review studies covering Ethiopia, Kenya, Malawi, Tanzania, Ghana, and Uganda was conducted. The studies employed qualitative (n = 5), mixed-methods (n = 1), cross-sectional survey (n = 1), and descriptive analysis (n = 1) approaches, with sample sizes ranging from 20–60 stakeholders, including policymakers and health professionals. Barriers and enablers were categorized into five themes: human resource capacity, financial and infrastructural constraints, policy and governance frameworks, stakeholder engagement and political will, and data and evidence availability.
Results: Seventeen barriers and sixteen enablers were identified. The key barriers included limited technical capacity (5 studies), financial constraints (4 studies), a lack of standardized HTA frameworks and guidelines (3 studies), political interference (1 study), limited evidence use (1 study), and cultural/legal challenges (1 study) The enablers included stakeholder engagement (3 studies), political will and UHC alignment (2 studies), capacity building (3 studies), legal/institutional frameworks (2 studies), international collaboration (2 studies), and transparent policymaking (1 study). Countries such as Kenya and Ethiopia have progressed through institutional structures and international support, while resource and governance challenges have persisted across contexts.
Conclusion: HTA adoption in Sub-Saharan Africa is hindered by human resource shortages, funding limitations, and weak governance, but facilitated by stakeholder engagement, political commitment, and international partnerships. Tailored interventions, including capacity building, sustainable financing, and standardized frameworks, are essential for institutionalizing HTA and advancing evidence-based health financing for UHC. Future research should explore underrepresented countries and employ longitudinal designs to increase generalizability.