
Preventing Rectal Toxicity in Prostate Cancer: Diet and Supplement Alternative to Enemas or Rectal Spacer
Radiation Therapy OncologyReceived 07 Feb 2024 Accepted 26 Mar 2024 Published online 27 Mar 2024
ISSN: 2995-8067 | Quick Google Scholar
Next Full Text
Threat to Human and Animal Health Caused by Mycotoxins and Masked Mycotoxins Occurring in Food and Feed
Previous Full Text
Breast Cancer: The Road to a Personalized Prevention


Received 07 Feb 2024 Accepted 26 Mar 2024 Published online 27 Mar 2024
Background: Rectal toxicity is an important side effect of prostate cancer irradiation affecting 25% of patients. The role of dosimetric variables has a set of dose-volume constraints and curves to estimate the risk of rectal damage. The rectum position at the time of CT planning is different from the position during radiotherapy. Three methods are available to achieve optimal rectum position: enema; prostate cancer spacer; fiber-/fat-free diet.
Methods: A 70.2 Gray radiation divided into 26 hypo-fractions was administered to 115 patients with prostate cancer by VMAT referred to a single center in Italy. To empty the rectum, all patients were administered a fiber-/fat-free diet and those with Eating Disorders (ED) were also added with activated charcoal (2 tablets/day) and a macrogol-based medical device (2 sachets/day). During treatment, the volumetric amount of rectum in the target was measured by comparing control-CT with simulation-CT, and acute toxicity was also checked.
Results: The rectum position during control-CT in diet-only patients (29) predicted toxicity recorded during treatment, while in the ED group rectum position was adherent to position during simulations. Rectal volume target > 0.25 cc receiving a dose > V70 caused acute G3 toxicity that attenuated or worsened with rectal displacement. Acute rectal toxicity occurred in 6/29 (20.68%) patients (1 G3, 5 G1) in the diet-only group, while only in 1/86 (1.16%) patients (G1) in the ED group. No chronic toxicity was recorded in either group.
Conclusion: Prostate cancer patients treated with VMAT, diet, charcoal, and macrogol emptied the rectum optimally and reduced incidence and severity of acute rectal toxicity, also with benefit on late toxicity.
The most common collateral effect of prostate cancer irradiation is rectal toxicity. It usually occurs in 25% of patients and it consists of changes in bowel habits from mild to moderate urgency, diarrhea-like stools, fecal incontinence, and bleeding. To avoid this, each patient’s Dose-Volume Histogram (DVH) is assessed before performing Radiotherapy (RT). If the radiation dose applied to the rectum exceeds the recommended dose, the dosing plan should be revised until collateral toxicity is avoided. There is growing evidence that acute injury precedes late toxicity [-], so identifying factors predictive of acute toxicity improves patients’ quality of life during and after RT and leads clinicians to personalize treatments.
Currently, in acute rectal toxicity, the role of dosimetric variables is quite well understood, as a robust set of dose-volume constraints and logistic curves estimating the associated risk of rectal damage is readily available [,]. One of the many issues faced is the position of the rectum, as at the time of Computer Tomography (CT) planning for radiotherapy its position is not fully representative of the one assumed during RT due to inter- or intra-fractional variations in rectal filling, intestinal gas, and bladder filling. This usually results in inappropriate radiation dose delivered to the rectum and in acute toxicity. An empty rectum during the simulation is desirable so as not to introduce a systematic error in the Planning Target Volume (PTV) coverage [].
From the above, rectal CT imaging characteristics before and especially during treatment can predict radiotoxicity. Therefore, the combination of imaging and clinical/dosimetric characteristics improves the predictive performance of the radiotoxicity model []. A high rate of acute rectal toxicity is associated with late RT proctopathy [,]. An always empty rectum both on CT scan and during treatment is a gold standard. To achieve this optimal condition there are at least three methods: to use every day the same preparation for rectoscopy; to introduce a spacer into the rectum; and to recommend a fat- and fiber-free diet to the patient. In daily CT controls this objective is not always achieved, with resulting toxicity. Despite the methods to achieve an empty rectum ready for RT may vary by center and by country, most radiotherapy teams agree to follow the National Comprehensive Cancer Network (NCCN) guidelines for the treatment of prostate cancer patients. In our center the NCCN guidelines version 2023 were followed at the time of this study, now updated to version 1.2024.
Specifically, very little has been published on the efficacy and toxicity of the current techniques used to empty the colon. The aim of this single-center study was to evaluate the efficiency of an innovative rectal emptying technique more suited to the age of patients affected by prostate cancer, to improve the understanding of how to easily and affordably avoid rectal toxicity, and to assess the results in reducing the colon radiation effects.
From April 2020 to December 2022, 70.2 Gray (Gy) dose radiation divided in 26 hypo-fraction was administered on the prostate and seminal vesicles according to Volumetric Modulated Arc Therapy (VMAT) technique to each of the 115 consecutive patients attending the Oncological Radiotherapy Unit at the Cosenza Hospital, Cosenza (Italy). The study has been tacitly approved by the institutional research ethics committee, as the research was based on data collected during clinical routine, without the adoption of any a priori research protocol, and has been conducted in accordance with the principles set forth in the Helsinki Declaration. Each patient enrolled in the present study gave his informed consent for participation in this research.
During the first visit, each patient in the study was warned about possible side effects related to RT and received an explanatory card on how to prepare both for the CT scan centering and for the entire treatment. All patients were given the diet, and subjects with Eating Disorders (ED) were also advised on activated charcoal and a macrogol-based medical device (AgPeg®). This additional treatment to the diet in ED patients consisted of a daily two charcoal tablets daily associated with two sachets of macrogol preparation. The goal of this first visit was to have patients with a partially empty rectum and a consistently full bladder during both preparation and RT. To avoid intestinal gas formation, the bladder was filled three hours before the treatment/simulation and the patient had to follow a fiber- and fat-free diet (Table 1).
After simulation, the DVH was accurately assessed to allow the patient to undergo the treatment according to the Radiation Therapy Oncology Group (RTOG) dose toxicity limits. During RT we measured the volume of the rectum that moved to the target, just by comparing the control CT (performed every day before treatment) versus the simulation CT. A further check on toxicity was carried out even in the presence of apparently perfect images, with the aim to detect side effects recorded during treatment and in the month after the end of radiotherapy. By combining clinical parameters with imaging findings (i.e., the amount of rectum entering the target and the acute toxicity), we were able to anticipate the patient’s development of acute rectal toxicity predictive of possible late chronic toxicity. The Common Terminology Criteria for Adverse Events version 3.0 was used to classify rectal toxicity [].
The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.
According to diet regimens followed during the trial, two groups of patients were studied: 29 subjects following a fiber- and fat-free diet only, and 86 subjects affected by ED and following the diet plus charcoal and macrogol supplementation (AgPeg®). The major patients’ demographic characteristics are reported in Table 2.
Measurement of the irradiated rectum during control CT along with bladder filling measurements in patients following the diet-only (Figure 1) proved to be predictive of the toxicity recorded during treatment. On the other side, in the group of patients with ED and treated with diet and charcoal + macrogol medical device, the irradiated rectum was perfectly adherent to the image of the rectum measured at the simulation time (Figure 2), and no toxicity was recorded. During measurements, the rectum tended to move towards the target only in the fiber- and fat-free diet-only group. A rectal volume entering the target more than 0.25 cubic centimeters (cc) and receiving a dose greater than V70 for several sessions developed acute G3 toxicity that attenuated or worsened as the rectum moved during the subsequent measurements solicited by the introduction of the spacer (SpaceOARTM Hydrogel) (Table 3) [,]. Acute rectal toxicity occurred in 6 out of 29 patients (20.68%) in the diet-only group (Table 4), while in the group with ED G1 acute toxicity was observed only in 1 out of 86 (1.16%) patients (Table 5). Only 3 patients in this last group reported diarrhea (3.48%) and for this reason, they suspended the supplementation without interruption of RT treatment, with immediate intestinal recovery and no acute toxicity. The dose/volume/irradiation time relationship is well-established and after more than 6 months from the end of RT, no chronic toxicity has been observed in either group due to this method that allowed to minimize or almost nullify the acute toxicity.
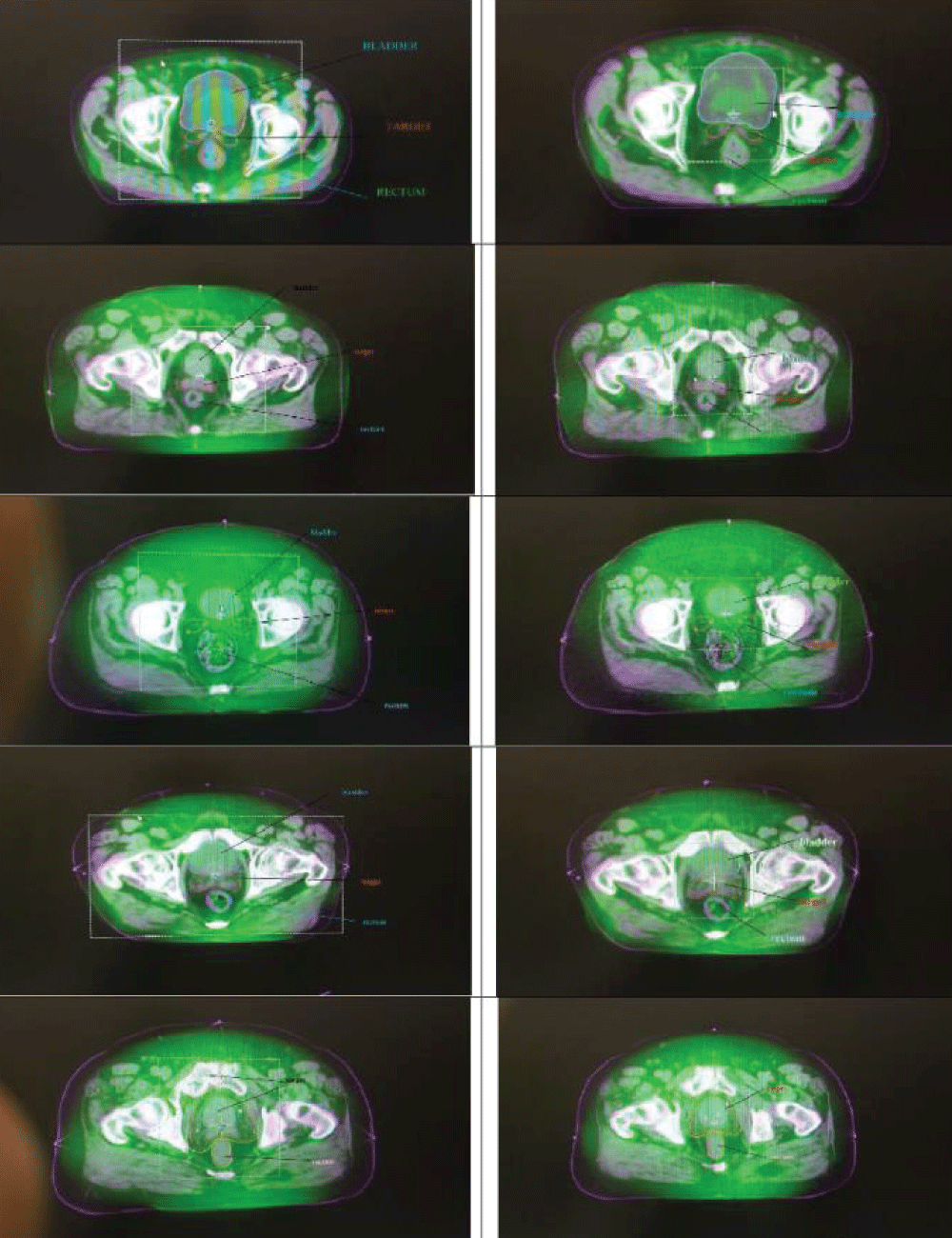 Figure 2: Cone Beam Computed Tomography (CBCT). Subjects with eating disorders (ED) following fiber-and fat-free diet + activated charcoal and macrogol-based medical device.
Figure 2: Cone Beam Computed Tomography (CBCT). Subjects with eating disorders (ED) following fiber-and fat-free diet + activated charcoal and macrogol-based medical device.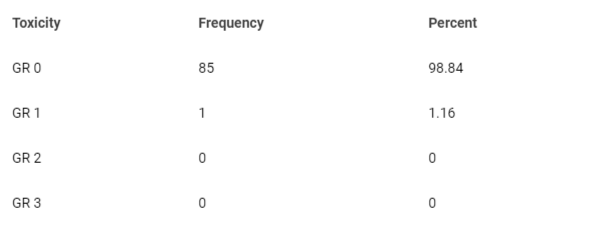 Table 5: Frequency of acute rectal toxicity in patients with ED following a fiber-free diet plus charcoal and macrogol.
Table 5: Frequency of acute rectal toxicity in patients with ED following a fiber-free diet plus charcoal and macrogol.According to: Lawrence B Marks, Ellen D Yorke, Andrew Jackson, Use of normal tissue complication probability models in the clinic Int J Radiat Oncol Biol Phys. 2010 Mar 1;76(3 Suppl):S10-9. doi: 10.1016/j.ijrobp.2009.07.1754
The follow-up of all patients has been performed according to the NCCN guidelines for cancer prostate [].
We analyzed the advantages and disadvantages of other techniques used to irradiate the rectum without toxicity [].
The rectal spacer, used to move the rectum away from the prostate and from a high dose of radiation, reduces any type of side effects the patient may experience during and after radiotherapy. Nevertheless, if the spacer is inserted incorrectly, for example into a blood vessel or into the rectum, the radiation oncologist will have to wait roughly three months before the procedure can be repeated until the body has absorbed the gel. Such a long delay in the administration of a radiotherapy session can have negative effects on the progression of prostate cancer. Besides, the spacer insertion has to be surgically performed under local anesthesia although fasting is not required, but it is helpful to have an empty rectum before the procedure. It is needed to pay attention to some patient’s concomitant medical therapy (e.g., antiplatelets, anticoagulants) that need to be suspended before and some days after insertion or to other drugs (e.g., antidiabetics, etc.). Before the surgical procedure, an antibiotic prophylaxis has to be administered, and a close teamwork with surgeons has to be planned. With this method there are several disadvantages and the area of irradiated rectum surprisingly increases compared to other methods even if the late toxicity ultimately does not change [,]. Biocompatible and biodegradable perirectal spacer materials may be implanted between the prostate and rectum in patients undergoing external radiotherapy with organ-confined prostate cancer in order to displace the rectum from high radiation dose regions for the purpose of toxicity reduction. Patients with grossly apparent posterior extra-prostatic extension should not undergo perirectal spacer implantation [].
An alternative and more frequently used method consists of a daily evacuating enema, useful for eliminating intestinal gas, increasing the water content in the stool, and emptying the rectum and/or the descending colon. Common enema solutions include normal saline, a mix of salt and water. The salt mixture draws water into the intestines to soften the stool, and the patient must follow special dietary instructions the days before the enema. This method is not highly appreciated by patients due to the diet and the discomfort of enema, both to be continued throughout the period of simulation and treatment. In elderly patients, weight loss can occur, and sometimes a liquid diet may be required.
Since it is mandatory the patient must have an empty rectum in order to achieve good radiotherapy treatment results, the first thing the radiation oncologist has to recommend is a low-fiber and low-fat diet, so that the rectum has a better emptying chance before treatment (this is routine in Italian Centres). After the first patients’ checks by control CT scan, we realized that something had to be added to the diet (Figure 1), such as vegetable charcoal, with the aim to reduce intestinal gas which inevitably forms in the rectum and macrogol, which draws water into the feces without interfering with the patient’s metabolic balance. In this way, we thought patients would not have suffered discomfort due to a long-lasting treatment of several weeks. In our experience, the only side effect due to this type of treatment was diarrhea observed in 3 patients (3.48%), which immediately regressed with the reduction or suspension of the recommended supplement without jeopardizing the benefit of the current radiotherapy treatment. Our method was safe and without serious complications.
In this experience we managed to combine two important aspects of prostate radiotherapy: the quality of irradiation and the quality of patient’s life. The gold standard of every specialist is to deliver the patient a high-quality irradiation, but this ideal aim often struggles with a reality that is very different from what is imagined. In the case of prostate treatment, the radiation area is close to two highly mobile organs: the bladder and the rectum. Filling the bladder a few hours before the treatment can help to prevent consequences.
Then, we studied how to gently empty the rectum without resorting to rectal spacers or other more powerful laxatives. Patients appreciated our new approach consisting of fiber- and fat-free diet associated with activated charcoal and macrogol-based medical device (AgPeg®). The use of vegetable charcoal and macrogol in addition to the diet has allowed the continuous elimination of faeces and gas, turning the rectum from a moving Organ at Risk (OAR) into a fixed OAR, without compromising its functionality. Thus, while in the past the effects of rectal toxicity were common and sometimes so severe to resort to an abdominal surgeon’s intervention, now the images have shown (Figure 2)
very clearly that the rectum does not move during the entire period from the onset to the end of the treatment.
Conversely, with the diet-only the rectal movement, albeit minimal, was present as well as some acute rectal toxicity. With the method consisting of the diet associated with vegetable charcoal and macrogol-based medical device followed in our experience, the patient did not interrupt the treatment and did not experience intestinal problems requiring medical interventions.
There is little literature on rectal toxicity. In the table published by Arcangeli [] only two authors [,] have highlighted how G2 rectal toxicity with IMRT (Intensity-modulated radiation therapy) uses computer-controlled x-ray linear accelerators to deliver accurate patient doses of radiation into malignant tumors. So, the delivered radiation dose to patients is more targeted to the three-dimensional shape of the tumor by modulating the intensity of the radiation beam. With VMAT the irradiation times are shorter and toxicity is smaller ranging from 5 to 22% in patients with all stages (low, intermediate, severe) of the disease. In our experience with patients in an intermediate stage of cancer disease, we observed lower toxicity. No other studies have been published on this topic because in clinical practice it is usually preferred to solve the problems resulting from the implantation of a rectal spacer, despite the limitations of the technique described [].
In the study of Porreca and colleagues, almost 5% of the 1,705 patients reported the use of at least one daily incontinence pad to control urinary loss. Less than 3% of patients reported moderate/severe problems related to bowel functions, and sexual function was a moderate/severe problem for 26.7% of subjects. Diabetes, more than other moderate/severe comorbidities, prostate cancer at T2 or T3-T4 stages, and Gleason score ≥8 were significantly associated with lower sexual function scores at diagnosis [].
In our study, the small number of studied subjects did not allow us to relate comorbidities to sexual function. As far as regards urinary toxicity, episodes of G2 cystitis were observed only in 20% of patients during treatment and were treated with supplements, while the use of diapers has not yet been reported to us.
In prostate cancer, patients treated with the Volumetric Modulated Arc Therapy (VMAT) schedule, the use of a diet supplemented by vegetable charcoal associated with a macrogol-based medical device lowered the incidence and degree of acute rectal toxicity better than diet alone. There were no cases of late toxicity in either group. This experience was provided with a large scale of patients, giving an accurate insight into rectal toxicity from VMAT in prostate cancer.
Our study suggests that a diet associated with these types of supplements reduces rectal movement with a clear benefit on acute and late toxicity and that bladder filling helps to avoid both complications. Continuous dialogue with patients promotes their compliance and improves the final result. Nevertheless, this study has some limitations: no calculation to determine the sample size of patients to be studied has been preliminary performed, and therefore no statistical comparison between groups has been applied; the study was performed in a single center and it was not possible to verify whether this new method can be exported to a larger population and with more homogeneous demographic characteristics; patients were not stratified according to their BMI to verify whether these indices can modify the results obtained. This study had only the aim of initially verifying whether the technique of combining a fat- and fiber-free diet with vegetal charcoal and a macrogol-based medical device produced an appreciable effect on the patient population attending our center.
Other studies are needed to confirm the results obtained from our experience, with a larger series of cases and more homogeneous groups in terms of disease stage, concomitant pathologies, and BMI.
Dörr W, Hendry JH. Consequential late effects in normal tissues. Radiother Oncol. 2001 Dec;61(3):223-31. doi: 10.1016/s0167-8140(01)00429-7. PMID: 11730991.
Jereczek-Fossa BA, Zerini D, Fodor C, Santoro L, Serafini F, Cambria R, Vavassori A, Cattani F, Garibaldi C, Gherardi F, Ferrari A, Rocco B, Scardino E, de Cobelli O, Orecchia R. Correlation between acute and late toxicity in 973 prostate cancer patients treated with three-dimensional conformal external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2010 Sep 1;78(1):26-34. doi: 10.1016/j.ijrobp.2009.07.1742. Epub 2010 Feb 3. PMID: 20133085.
Lock M, Best L, Wong E, Bauman G, D'Souza D, Venkatesan V, Sexton T, Ahmad B, Izawa J, Rodrigues G. A Phase II trial of arc-based hypofractionated intensity-modulated radiotherapy in localized prostate cancer. Int J Radiat Oncol Biol Phys. 2011 Aug 1;80(5):1306-15. doi: 10.1016/j.ijrobp.2010.04.054. Epub 2010 Aug 12. PMID: 20708855.
Cella L, D'Avino V, Liuzzi R, Conson M, Doria F, Faiella A, Loffredo F, Salvatore M, Pacelli R. Multivariate normal tissue complication probability modeling of gastrointestinal toxicity after external beam radiotherapy for localized prostate cancer. Radiat Oncol. 2013 Sep 23;8:221. doi: 10.1186/1748-717X-8-221. PMID: 24053357; PMCID: PMC3852304.
Fiorino C, Valdagni R, Rancati T, Sanguineti G. Dose-volume effects for normal tissues in external radiotherapy: pelvis. Radiother Oncol. 2009 Nov;93(2):153-67. doi: 10.1016/j.radonc.2009.08.004. Epub 2009 Sep 16. PMID: 19765845.
Michalski JM, Gay H, Jackson A, Tucker SL, Deasy JO. Radiation dose-volume effects in radiation-induced rectal injury. Int J Radiat Oncol Biol Phys. 2010 Mar 1;76(3 Suppl):S123-9. doi: 10.1016/j.ijrobp.2009.03.078. Erratum in: Int J Radiat Oncol Biol Phys. 2019 Aug 1;104(5):1185. PMID: 20171506; PMCID: PMC3319467.
Mostafaei S, Abdollahi H, Kazempour Dehkordi S, Shiri I, Razzaghdoust A, Zoljalali Moghaddam SH, Saadipoor A, Koosha F, Cheraghi S, Mahdavi SR. CT imaging markers to improve radiation toxicity prediction in prostate cancer radiotherapy by stacking regression algorithm. Radiol Med. 2020 Jan;125(1):87-97. doi: 10.1007/s11547-019-01082-0. Epub 2019 Sep 24. PMID: 31552555.
Denham JW, O'Brien PC, Dunstan RH, Johansen J, See A, Hamilton CS, Bydder S, Wright S. Is there more than one late radiation proctitis syndrome? Radiother Oncol. 1999 Apr;51(1):43-53. doi: 10.1016/s0167-8140(99)00027-4. PMID: 10386716.
Heemsbergen WD, Peeters ST, Koper PC, Hoogeman MS, Lebesque JV. Acute and late gastrointestinal toxicity after radiotherapy in prostate cancer patients: consequential late damage. Int J Radiat Oncol Biol Phys. 2006 Sep 1;66(1):3-10. doi: 10.1016/j.ijrobp.2006.03.055. Epub 2006 Jul 11. PMID: 16814954.
Common Terminology Criteria for Adverse Events (CTCAE) version 3.0 Web site [cited 2016 Dec 4]. https://ctep.cancer.gov/protocol development/electronic_applications/docs/ctcaev3.pdf.
Marks LB, Yorke ED, Jackson A, Ten Haken RK, Constine LS, Eisbruch A, Bentzen SM, Nam J, Deasy JO. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 2010 Mar 1;76(3 Suppl):S10-9. doi: 10.1016/j.ijrobp.2009.07.1754. PMID: 20171502; PMCID: PMC4041542.
Ozkan EE, Ozseven A, Cerkesli ZAK. Evaluating the predictive value of quantec rectum tolerance dose suggestions on acute rectal toxicity in prostate carcinoma patients treated with IMRT. Rep Pract Oncol Radiother. 2020 Jan-Feb;25(1):50-54. doi: 10.1016/j.rpor.2019.12.002. Epub 2019 Dec 9. PMID: 31889921; PMCID: PMC6931199.
Arcangeli S, Greco C. Hypofractionated radiotherapy for organ-confined prostate cancer: is less more? Nat Rev Urol. 2016 Jul;13(7):400-8. doi: 10.1038/nrurol.2016.106. Epub 2016 Jun 14. PMID: 27296648.
Storey MR, Pollack A, Zagars G, Smith L, Antolak J, Rosen I. Complications from radiotherapy dose escalation in prostate cancer: preliminary results of a randomized trial. Int J Radiat Oncol Biol Phys. 2000 Oct 1;48(3):635-42. doi: 10.1016/s0360-3016(00)00700-8. PMID: 11020558.
Huang EH, Pollack A, Levy L, Starkschall G, Dong L, Rosen I, Kuban DA. Late rectal toxicity: dose-volume effects of conformal radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2002 Dec 1;54(5):1314-21. doi: 10.1016/s0360-3016(02)03742-2. PMID: 12459352.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Prostate Cancer Version 1. 2024.
Kuban DA, Nogueras-Gonzalez GM, Hamblin L, Lee AK, Choi S. Preliminary Report of a Randomized Dose Escalation Trial for Prostate Cancer using Hypofractionation. Int J Radiat Oncol Biol Phys2010; 78:S58–S59.
Pollack A, Walker G, Horwitz EM, Price R, Feigenberg S, Konski AA, Stoyanova R, Movsas B, Greenberg RE, Uzzo RG, Ma C, Buyyounouski MK. Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol. 2013 Nov 1;31(31):3860-8. doi: 10.1200/JCO.2013.51.1972. Epub 2013 Oct 7. PMID: 24101042; PMCID: PMC3805927.
Porreca A, Noale M, Artibani W, Bassi PF, Bertoni F, Bracarda S, Conti GN, Corvò R, Gacci M, Graziotti P, Magrini SM, Mirone V, Montironi R, Muto G, Pecoraro S, Ricardi U, Russi E, Tubaro A, Zagonel V, Crepaldi G, Maggi S; Pros-IT CNR study group. Disease-specific and general health-related quality of life in newly diagnosed prostate cancer patients: the Pros-IT CNR study. Health Qual Life Outcomes. 2018 Jun 13;16(1):122. doi: 10.1186/s12955-018-0952-5. PMID: 29898750; PMCID: PMC6001046.
Piro F, Cosentino D, Piro U, Tocci G, Marafioti L. Preventing Rectal Toxicity in Prostate Cancer: Diet and Supplement Alternative to Enemas or Rectal Spacer. IgMin Res. Mar 27, 2024; 2(3): 171-0. IgMin ID: igmin161; DOI: 10.61927/igmin161; Available at: igmin.link/p161
Anyone you share the following link with will be able to read this content:
Address Correspondence:
Fabrizio Piro, Complex Operational Unit of Oncological Radiotherapy, Oncohaematological Department, Cosenza Hospital, Via San Martino snc, 87100, Cosenza, Italy, Email: [email protected]
How to cite this article:
Piro F, Cosentino D, Piro U, Tocci G, Marafioti L. Preventing Rectal Toxicity in Prostate Cancer: Diet and Supplement Alternative to Enemas or Rectal Spacer.
IgMin Res. Mar 27, 2024; 2(3): 171-0. IgMin ID: igmin161; DOI: 10.61927/igmin161; Available at: igmin.link/p161
Copyright: © 2024 Piro F, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
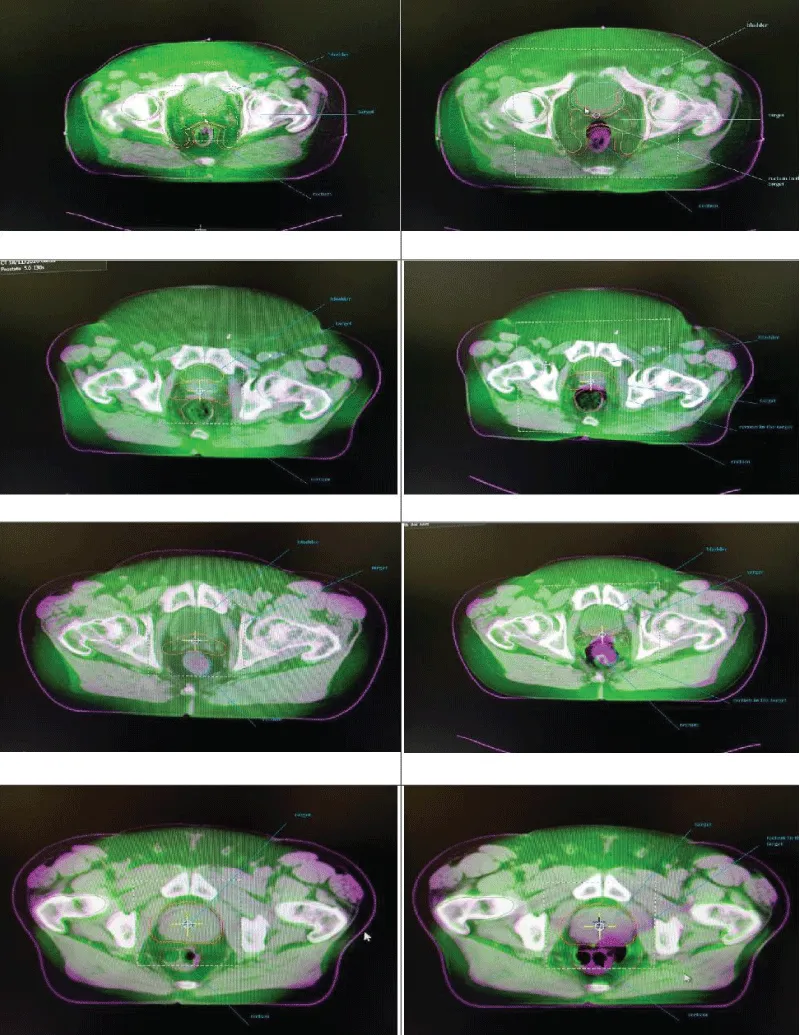 Figure 1: Cone Beam Computed Tomography (CBCT). Subjects fol...
Figure 1: Cone Beam Computed Tomography (CBCT). Subjects fol...
 Figure 2: Cone Beam Computed Tomography (CBCT). Subjects wit...
Figure 2: Cone Beam Computed Tomography (CBCT). Subjects wit...
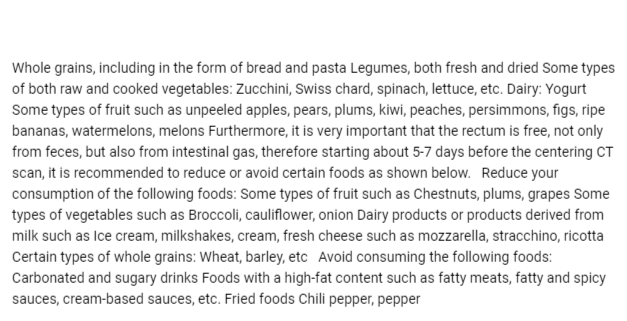 Table 1: The diet. A simplified list of foods conducive to ...
Table 1: The diet. A simplified list of foods conducive to ...
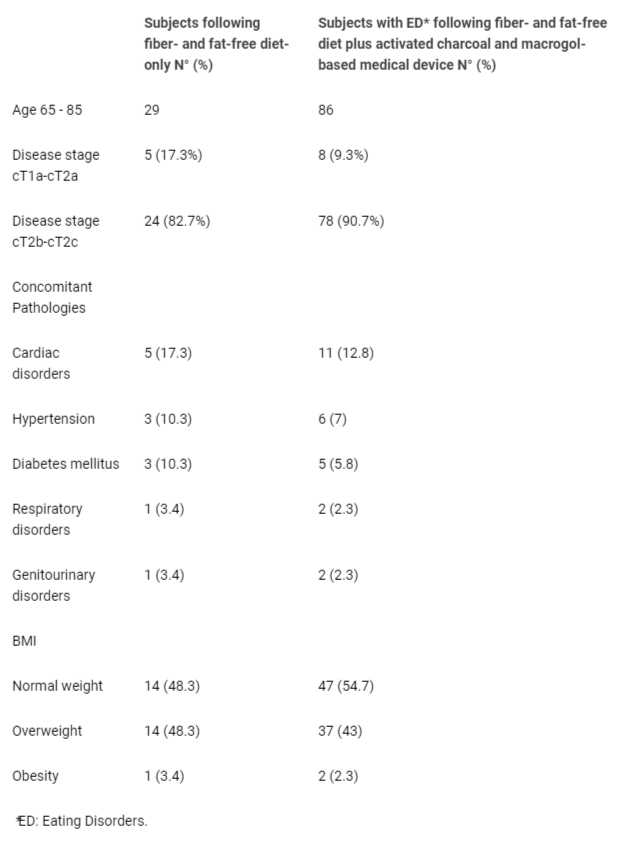 Table 2: Patient characteristics....
Table 2: Patient characteristics....
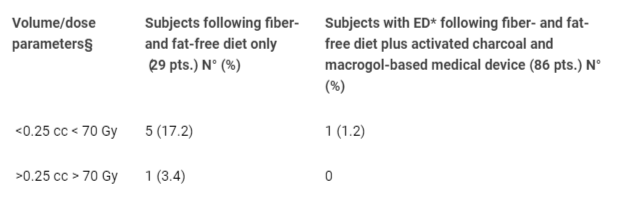 Table 3: Changes of position and radiation of the rectum du...
Table 3: Changes of position and radiation of the rectum du...
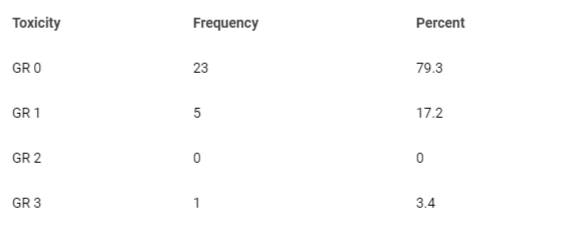 Table 4: Frequency of acute rectal toxicity in patients wit...
Table 4: Frequency of acute rectal toxicity in patients wit...
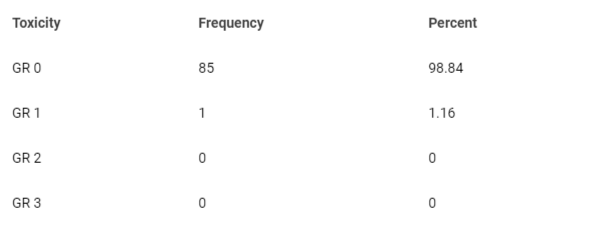 Table 5: Frequency of acute rectal toxicity in patients wit...
Table 5: Frequency of acute rectal toxicity in patients wit...
Dörr W, Hendry JH. Consequential late effects in normal tissues. Radiother Oncol. 2001 Dec;61(3):223-31. doi: 10.1016/s0167-8140(01)00429-7. PMID: 11730991.
Jereczek-Fossa BA, Zerini D, Fodor C, Santoro L, Serafini F, Cambria R, Vavassori A, Cattani F, Garibaldi C, Gherardi F, Ferrari A, Rocco B, Scardino E, de Cobelli O, Orecchia R. Correlation between acute and late toxicity in 973 prostate cancer patients treated with three-dimensional conformal external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2010 Sep 1;78(1):26-34. doi: 10.1016/j.ijrobp.2009.07.1742. Epub 2010 Feb 3. PMID: 20133085.
Lock M, Best L, Wong E, Bauman G, D'Souza D, Venkatesan V, Sexton T, Ahmad B, Izawa J, Rodrigues G. A Phase II trial of arc-based hypofractionated intensity-modulated radiotherapy in localized prostate cancer. Int J Radiat Oncol Biol Phys. 2011 Aug 1;80(5):1306-15. doi: 10.1016/j.ijrobp.2010.04.054. Epub 2010 Aug 12. PMID: 20708855.
Cella L, D'Avino V, Liuzzi R, Conson M, Doria F, Faiella A, Loffredo F, Salvatore M, Pacelli R. Multivariate normal tissue complication probability modeling of gastrointestinal toxicity after external beam radiotherapy for localized prostate cancer. Radiat Oncol. 2013 Sep 23;8:221. doi: 10.1186/1748-717X-8-221. PMID: 24053357; PMCID: PMC3852304.
Fiorino C, Valdagni R, Rancati T, Sanguineti G. Dose-volume effects for normal tissues in external radiotherapy: pelvis. Radiother Oncol. 2009 Nov;93(2):153-67. doi: 10.1016/j.radonc.2009.08.004. Epub 2009 Sep 16. PMID: 19765845.
Michalski JM, Gay H, Jackson A, Tucker SL, Deasy JO. Radiation dose-volume effects in radiation-induced rectal injury. Int J Radiat Oncol Biol Phys. 2010 Mar 1;76(3 Suppl):S123-9. doi: 10.1016/j.ijrobp.2009.03.078. Erratum in: Int J Radiat Oncol Biol Phys. 2019 Aug 1;104(5):1185. PMID: 20171506; PMCID: PMC3319467.
Mostafaei S, Abdollahi H, Kazempour Dehkordi S, Shiri I, Razzaghdoust A, Zoljalali Moghaddam SH, Saadipoor A, Koosha F, Cheraghi S, Mahdavi SR. CT imaging markers to improve radiation toxicity prediction in prostate cancer radiotherapy by stacking regression algorithm. Radiol Med. 2020 Jan;125(1):87-97. doi: 10.1007/s11547-019-01082-0. Epub 2019 Sep 24. PMID: 31552555.
Denham JW, O'Brien PC, Dunstan RH, Johansen J, See A, Hamilton CS, Bydder S, Wright S. Is there more than one late radiation proctitis syndrome? Radiother Oncol. 1999 Apr;51(1):43-53. doi: 10.1016/s0167-8140(99)00027-4. PMID: 10386716.
Heemsbergen WD, Peeters ST, Koper PC, Hoogeman MS, Lebesque JV. Acute and late gastrointestinal toxicity after radiotherapy in prostate cancer patients: consequential late damage. Int J Radiat Oncol Biol Phys. 2006 Sep 1;66(1):3-10. doi: 10.1016/j.ijrobp.2006.03.055. Epub 2006 Jul 11. PMID: 16814954.
Common Terminology Criteria for Adverse Events (CTCAE) version 3.0 Web site [cited 2016 Dec 4]. https://ctep.cancer.gov/protocol development/electronic_applications/docs/ctcaev3.pdf.
Marks LB, Yorke ED, Jackson A, Ten Haken RK, Constine LS, Eisbruch A, Bentzen SM, Nam J, Deasy JO. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 2010 Mar 1;76(3 Suppl):S10-9. doi: 10.1016/j.ijrobp.2009.07.1754. PMID: 20171502; PMCID: PMC4041542.
Ozkan EE, Ozseven A, Cerkesli ZAK. Evaluating the predictive value of quantec rectum tolerance dose suggestions on acute rectal toxicity in prostate carcinoma patients treated with IMRT. Rep Pract Oncol Radiother. 2020 Jan-Feb;25(1):50-54. doi: 10.1016/j.rpor.2019.12.002. Epub 2019 Dec 9. PMID: 31889921; PMCID: PMC6931199.
Arcangeli S, Greco C. Hypofractionated radiotherapy for organ-confined prostate cancer: is less more? Nat Rev Urol. 2016 Jul;13(7):400-8. doi: 10.1038/nrurol.2016.106. Epub 2016 Jun 14. PMID: 27296648.
Storey MR, Pollack A, Zagars G, Smith L, Antolak J, Rosen I. Complications from radiotherapy dose escalation in prostate cancer: preliminary results of a randomized trial. Int J Radiat Oncol Biol Phys. 2000 Oct 1;48(3):635-42. doi: 10.1016/s0360-3016(00)00700-8. PMID: 11020558.
Huang EH, Pollack A, Levy L, Starkschall G, Dong L, Rosen I, Kuban DA. Late rectal toxicity: dose-volume effects of conformal radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2002 Dec 1;54(5):1314-21. doi: 10.1016/s0360-3016(02)03742-2. PMID: 12459352.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Prostate Cancer Version 1. 2024.
Kuban DA, Nogueras-Gonzalez GM, Hamblin L, Lee AK, Choi S. Preliminary Report of a Randomized Dose Escalation Trial for Prostate Cancer using Hypofractionation. Int J Radiat Oncol Biol Phys2010; 78:S58–S59.
Pollack A, Walker G, Horwitz EM, Price R, Feigenberg S, Konski AA, Stoyanova R, Movsas B, Greenberg RE, Uzzo RG, Ma C, Buyyounouski MK. Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol. 2013 Nov 1;31(31):3860-8. doi: 10.1200/JCO.2013.51.1972. Epub 2013 Oct 7. PMID: 24101042; PMCID: PMC3805927.
Porreca A, Noale M, Artibani W, Bassi PF, Bertoni F, Bracarda S, Conti GN, Corvò R, Gacci M, Graziotti P, Magrini SM, Mirone V, Montironi R, Muto G, Pecoraro S, Ricardi U, Russi E, Tubaro A, Zagonel V, Crepaldi G, Maggi S; Pros-IT CNR study group. Disease-specific and general health-related quality of life in newly diagnosed prostate cancer patients: the Pros-IT CNR study. Health Qual Life Outcomes. 2018 Jun 13;16(1):122. doi: 10.1186/s12955-018-0952-5. PMID: 29898750; PMCID: PMC6001046.